Screening for Disease
Primary prevention: intervening in an asymptomatic person to prevent the onset of disease
Secondary prevention: using screening tests to identify pre-clinical disease in an asymptomatic person
Tertiary prevention: intervening in a person with known disease to prevent recurrence, complications, or worsening of that disease Screening targets an entire population or subpopulation of asymptomatic persons.
Key Criteria in the Decision to Screen, Ten criteria for effective screening: their application to multislice CT screening for pulmonary and colorectal cancers. Anderman, et al. Bulletin of the World Health Organization
Two ways to study a screening test: How accurate is it? Does its use in a screening program provide net benefit (reduced mortality without too much harm).
special challenges related to screening programs and their evaluation:
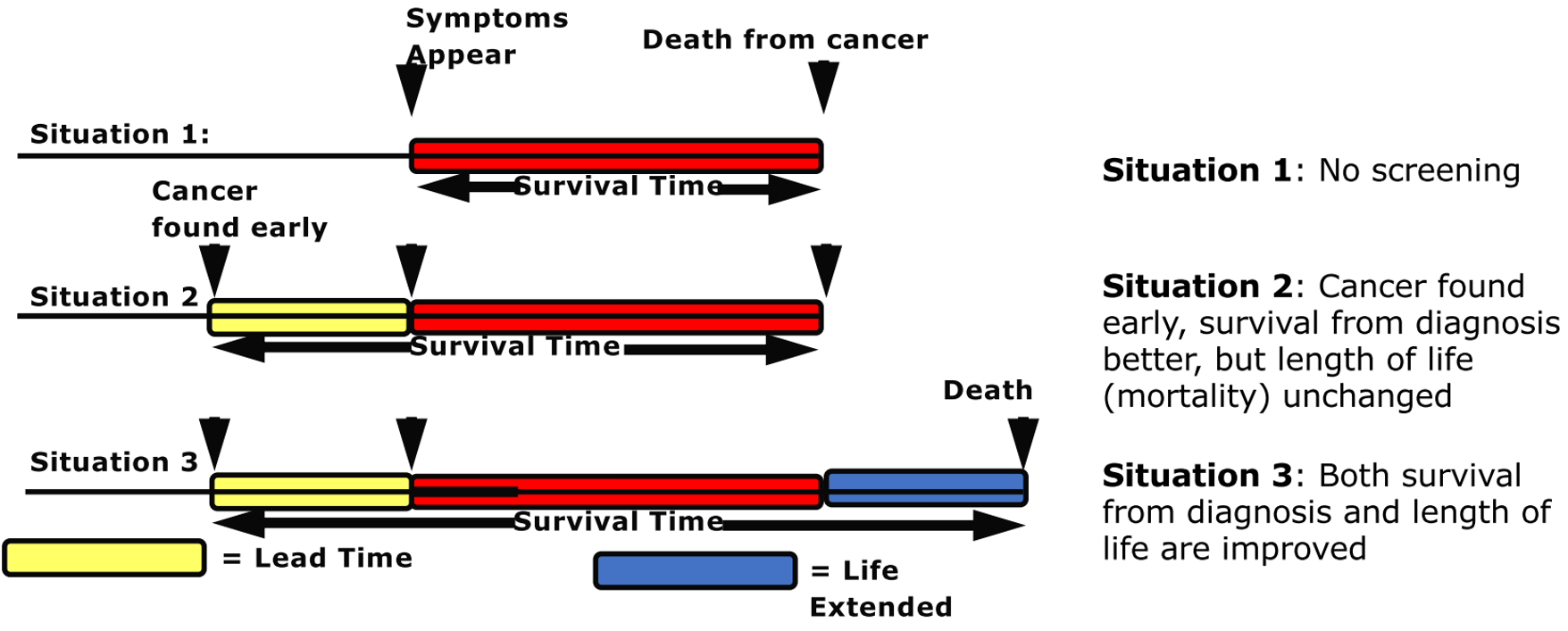
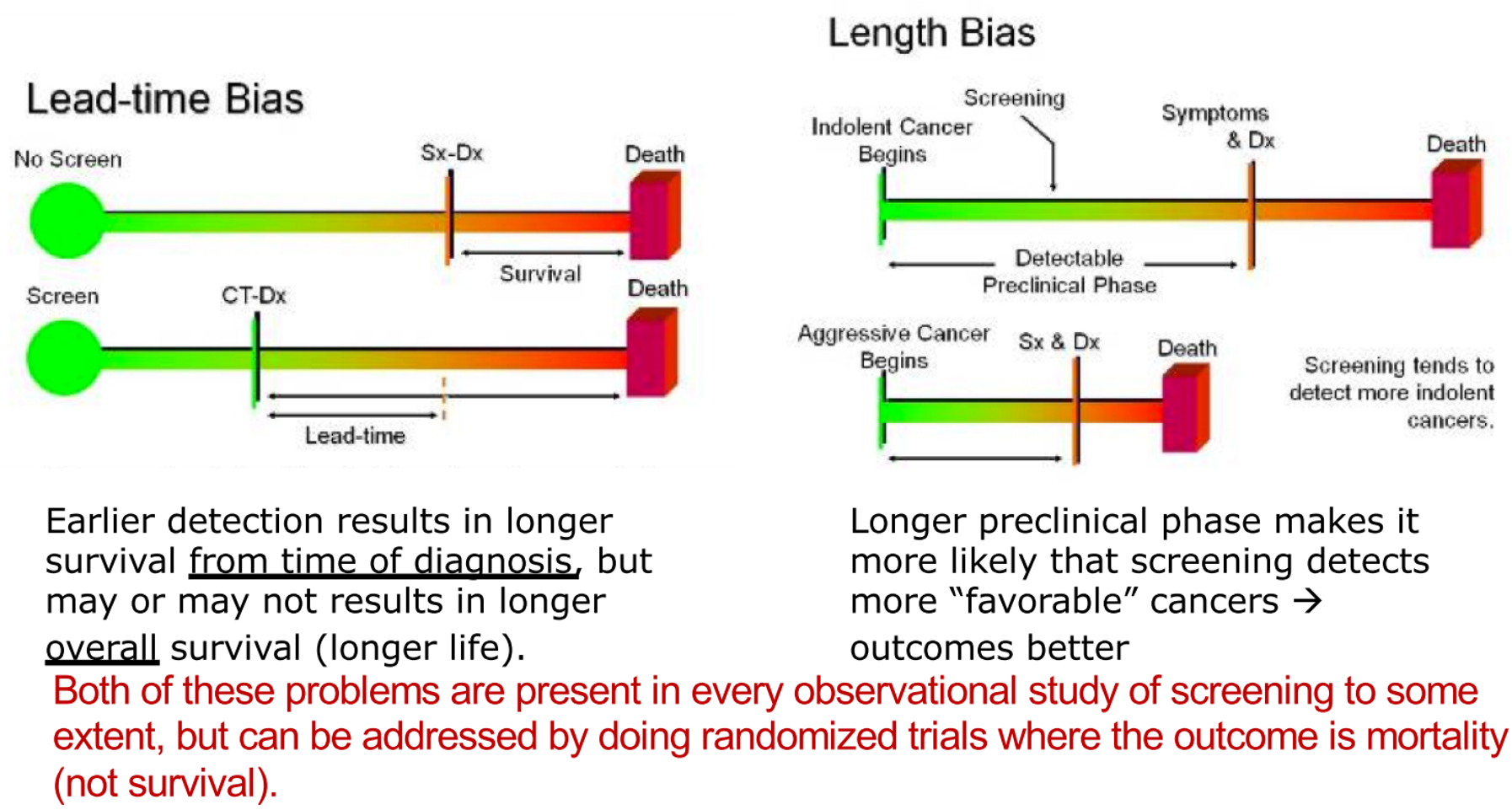
- Lead time bias: mortality or 5 year survival?: Survival is the time from diagnosis, mortality is time from birth. Survival from time of diagnosis is always prolonged by early detection. But that does not mean that death has been delayed or lives have been saved.
- Length time bias.
-
Healthy volunteer bias.
-
Cost and cost-effectiveness.
-
Overdiagnosis:
Rethinking screening for breast cancer and prostate cancer.
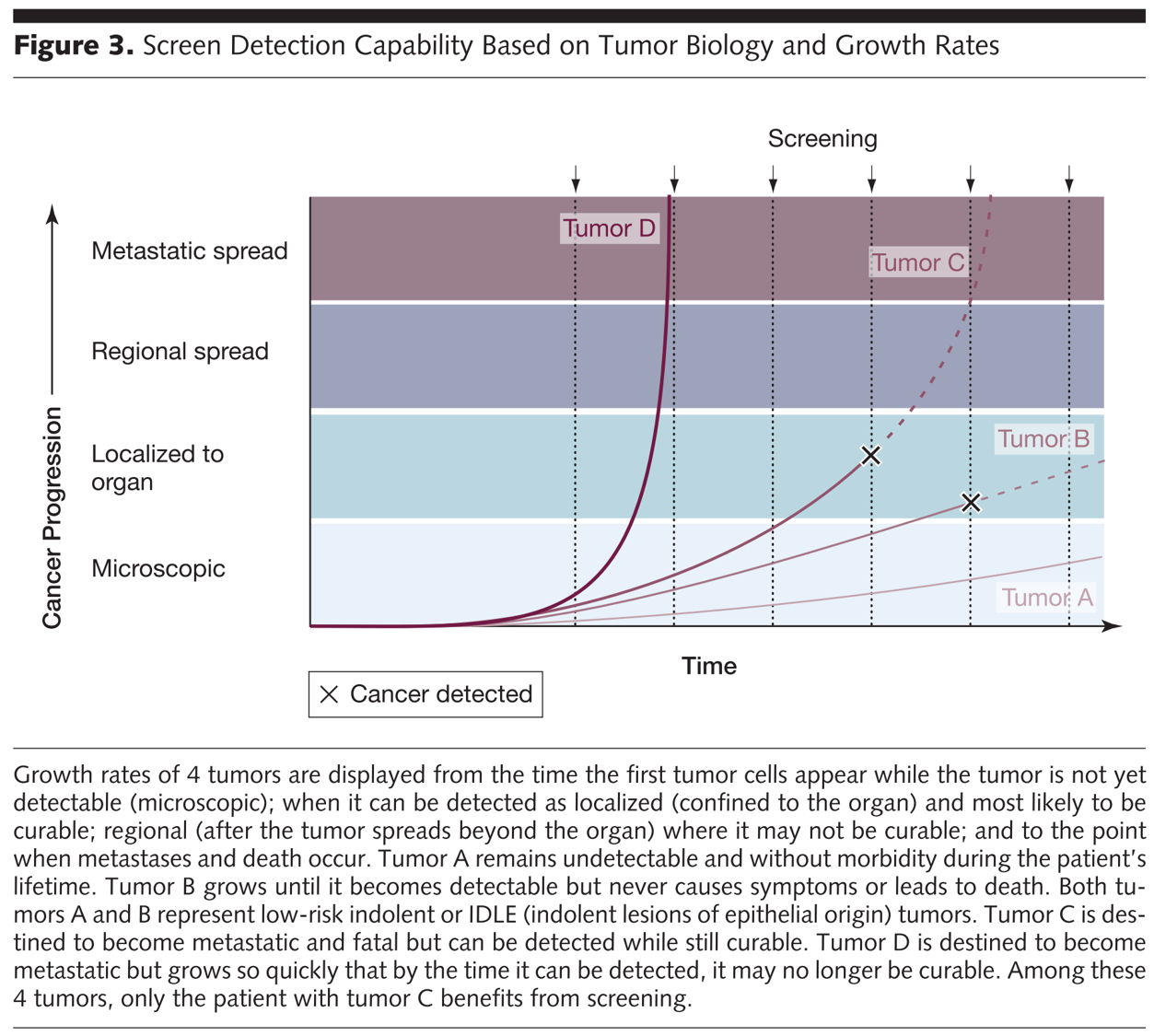
Conceptualizing overdiagnosis in cancer screening
Types of overdiagnosis: Tumor – Patient Classification: Tumor A: Asymptomatic malignant disease that regresses spontaneously if left alone (neuroblastoma). Tumor B: Asymptomatic malignant disease that either stagnates or progresses too slowly to be life threatening in even the longest of lifetimes (prostate cancer). Patient: Asymptomatic malignant disease that progresses quickly enough to be life threatening during a lifetime of typical length, but death because of another cause occurs prior to what would have been the destined date of symptomatic diagnosis had screening not occurred (lung cancer)
- Complexity of screening programs
We should screen when there is a net benefit (more benefit than harm). We also have to make sure disease is common enough to invest resources in screening, which can be expensive.
What about stopping? If disease is no longer common enough. If the person has an expected lifespan less than typical duration from screen detected to clinically detected disease. If the harms of treatment are likely to outweigh potential benefits.