Threshold model of decision-making
Definitions:
-
Primary care physicians (“generalists”). Physicians specializing in Family Medicine (all ages), Internal Medicine (adults only), and Pediatrics (kids only). In Europe/UK, general practitioners (“GPs”) provide primary care to all ages. Primary care is first contact care that is comprehensive, with continuity, across a range of ages and to both sexes. Includes focus on initial evaluation of clinical problems, management of chronic disease, preventive services, and without a limit based on organ system
-
Specialists (“Partialists”). Cardiology, gastroenterology, nephrology, infectious disease, dermatology, general surgery, ophthalmology, OB/Gyn, psychiatry. Focus is on a specific part of the body.
-
Diagnosis. Classifying the cause of signs and symptoms – why are they sick? Signs: what we detect on physical exam (e.g. crackles in the lungs, heart murmur, unequal pupils). Symptoms: what patients tell us or experience (e.g. cough, headache, throat hurts).
-
Treatment. An intervention intended to provide more benefit than harm to a person with an illness or health condition (e.g. surgery, medicine, therapy).
-
Prognosis. What is going to happen to someone with disease over time (e.g. 5 year survival rate).
-
Screening. Performing tests in an asymptomatic person to detect a disease (e.g. mammography screening to detect breast cancer)
-
Chief Complaint. The patient’s primary reason for seeing the doctor, such as chest pain, cough, or refill of medications.
The Clinical Process:
Some background on how physicians work and think. A patient presents to a physician with a complaint or symptom: Key tasks -> Negotiate a management plan.
Chief complaint
- Why are they here?
Diagnosis: Getting from a differential to a provisional diagnosis. Provisional diagnosis: what seems most likely at this point. Rule-out diagnosis: something important that has not been eliminated yet.
-
What don’t they have (ie something really bad), what might they have, and how can I narrow the possibilities?
-
Do they need any tests? In office, Ordered from elsewhere
Treatment
- How should they be treated initially?
Prognosis
-
What can they expect?
-
Do they require follow-up? If so, when?
Example: Taking a history of a patient with bowel problems
Example: Differential diagnosis. Patient with chest pain. What would you ask?
| Common | Uncommon | Rare |
|---|---|---|
| Musculoskeletal | Heart disease | Thoracic aneurysm |
| Anxiety disorder | Pulmonary embolism | Pulmonary abscess |
| Acid reflux (GERD) | Pneumonia | Subphrenic abscess |
| Costochondritis | Aortic stenosis | |
| Tuberculosis | ||
| Lung cancer |
Diagnostic strategies:
-
Pattern recognition or “Type 1 thinking”: Rapid recognition of patterns, rashes, classic symptoms or signs of disease.
-
Hypotheticodeductive or “Type 2 thinking”: Like a detective; Ask a series of questions and narrow down the diagnosis; Goal is to rule out all but one diagnosis by systematically asking a series of questions.
-
Algorithmic: order some tests, and use an algorithm to evaluate the tests.
Threshold Model
Developed by Pauker and Kassirer, 1980. To (eventually) rule-out or rule-in everything on the differential diagnosis list.
Key points to understanding the diagram:
-
Probability of disease ranges from 0% to 100%.
-
Below test threshold, disease is “ruled out” (at least for now).
-
Above the treatment threshold, we should “rule in” disease and start treatment.
-
Between thresholds, we need more information
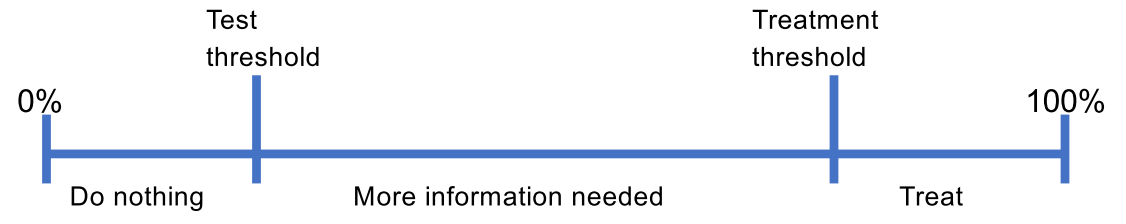
Questions: How are thresholds determined? How do we get more information?